With increasing life expectancy, age-related diseases are also on the rise. Primary arthrosis in the foot - i.e. degenerative wear and tear of the joints in particularly predisposed and stressed areas of the foot - is one of the typical diseases of old age. In some cases, however, factors unrelated to age can also trigger foot arthrosis (secondary arthrosis). In this article, you will learn everything about the most important issues surrounding the topic of arthrosis in the foot.
Navigate to the individual points here:
- Osteoarthritis: not only fingers and knees can be affected by the joint disease
- The different types of arthritis in the foot
- These symptoms often occur with arthrosis in the foot
- What causes arthrosis in the foot?
- How the Doctor diagnoses arthrosis in the foot
- In these cases, the foot surgeon considers an operation for arthrosis in the foot to be advisable
- What is the healing process like after the surgery?
- When are conservative treatment options for arthrosis of the foot really promising?
- Can arthrosis in the foot be prevented?
Osteoarthritis: not only fingers and knees can be affected by the joint disease
Over 140 joints ensure the human body's ability to move. The six major ones include the shoulder, elbow, hand, hip, knee and ankle joints. Injuries or signs of wear and tear can occur in these particularly stressed areas. In addition to the knee and finger joints, the ankles are also frequently affected by osteoarthritis - the breakdown of the cartilage layer between the joint bones.
What is arthrosis?
Arthrosis (arthrosis deformans, mechanical arthrosis, osteoarthrosis) is one of the most common joint diseases. The progressive, degenerative disease of the joint cartilage develops in different stages. Symptoms can range from mild joint stiffness to significantly limited joint mobility and severe pain.
In the course of the disease, the articular cartilage becomes structurally and functionally impaired, leading to deformation of the joints. In the course of the disease, the tissue underneath the bone changes. Here, pseudocysts or pathological proliferation of the bone substance inwards (hyperostosis) or outwards (exostoses) can develop due to remodelling processes.
The joint capsule tissue is also frequently affected. At this point, inflammation of the joint mucosa (synovitis) or a pathological increase in connective tissue (fibrosis) can occur.
Osteoarthritis most commonly affects the knee and finger joints. However, it can also occur in various parts of the foot.
What happens during the course of arthrosis in the foot?
In a healthy joint, the ends of the bones are covered with a protective layer of cartilage. This rubber-like material acts as the body's own shock absorber between the joint bones. With arthrosis in the foot, the robust cartilage mass gradually recedes until the bones rub directly against each other.
What are the consequences of arthrosis in the foot?
In the course of degenerative joint wear, inflammation, severe pain, bone outgrowths and increasingly limited freedom of movement occur.
The different types of arthritis in the foot
Do you notice changes in the big toe or other parts of the foot? Do you suffer from pain and limited mobility of the joints? Then arthrosis in the foot may be the cause. Arthrosis of the foot occurs particularly frequently in these three regions of the foot:
- Hallux rigidus - Here, the metatarsophalangeal joint of the big toe is affected by arthritis.
- Ankle joint arthrosis - The cartilage wear is located in the area of the ankle joint.
- Tarsal osteoarthritis - Cartilage degradation occurs at the tarsus or metatarsus.
Hallux rigidus refers to arthritis in the metatarsophalangeal joint of the big toe
A very common form of foot arthrosis is the so-called hallux rigidus. This arthrosis of the metatarsophalangeal joint of the big toe causes pain in the big toe, which is often noticeable when stepping and rolling and is accompanied by an increasing restriction of movement. General strain pain and inflammation of the big toe are further symptoms that increase over time as hallux rigidus progresses.
Arthrosis in the metatarsophalangeal joint of the big toe is usually caused by age, static problems, anatomical peculiarities, metabolic disorders or rheumatic diseases that lead to wear and tear of the joint cartilage in this highly stressed area of the foot.
This is how arthrosis of the ankle joint (joint degeneration) manifests itself
Like all joints, the ankle joint has a layer of cartilage that serves as a suspension and shock absorber. Ankle joint arthrosis occurs either due to the natural wear and tear of this cartilage or due to injuries that frequently occur at this point of the foot.
Malpositions that result in excessive wear of the joint can also be the cause. The first symptoms are often deep-seated pain in the ankle joint. In the further course of ankle joint arthrosis, morning start-up pain and general pain on exertion are typical.
The first symptoms can be deep-seated pain in the ankle joint. As ankle arthrosis progresses, morning start-up pain and general pain on exertion are typical.
Tarsal arthrosis occurs on the metatarsus
Arthrosis in the tarsus or metatarsus occurs rather rarely. But this form of joint wear and tear is also usually caused by age-related wear and tear and overloading. The buffering cartilage layer at the joints recedes, so that the joint bones rub against each other in the course of the disease. Considerable pain and reduced mobility are the consequences of tarsal arthrosis.
These symptoms often occur with arthrosis in the foot
General symptoms of osteoarthritis are pulling or stabbing pain in the affected region. Other very typical symptoms are pain when starting up or when straining, as well as joint stiffness and a reduced ability to move. But pain at rest can also occur.
Typical symptoms of arthrosis in the foot:
- Pain on the top of the foot or the back of the foot.
- stabbing pain when putting on and rolling off the foot
- Pain during and after continuous exertion, e.g. when walking
- Pressure pain when touching the top of the foot
- painful tarnishing after sitting for a long time
- morning start-up pain
- nocturnal rest pain
- greater sensitivity to the weather in the foot
- Warm sensation
- Evasive movement via heel or outside of the foot
- Deformations of the foot
With ankle joint arthrosis, additional symptoms may occur, such as:
- Swelling of the ankle joint
- Malalignment of the ankle joint
- radiating pain to the lower leg
If you notice symptoms that point to arthrosis in the foot, you are in particularly competent hands with foot surgeon Dr Tonio Gottlieb, MD. As an experienced foot specialist, he keeps the whole person and their body statics in mind during every treatment. Dr Gottlieb, MD has been researching foot diseases for many years. His therapies have international top quality and are scientifically up to date. See Dr Gottlieb's expertise for yourself and make an appointment for an examination.
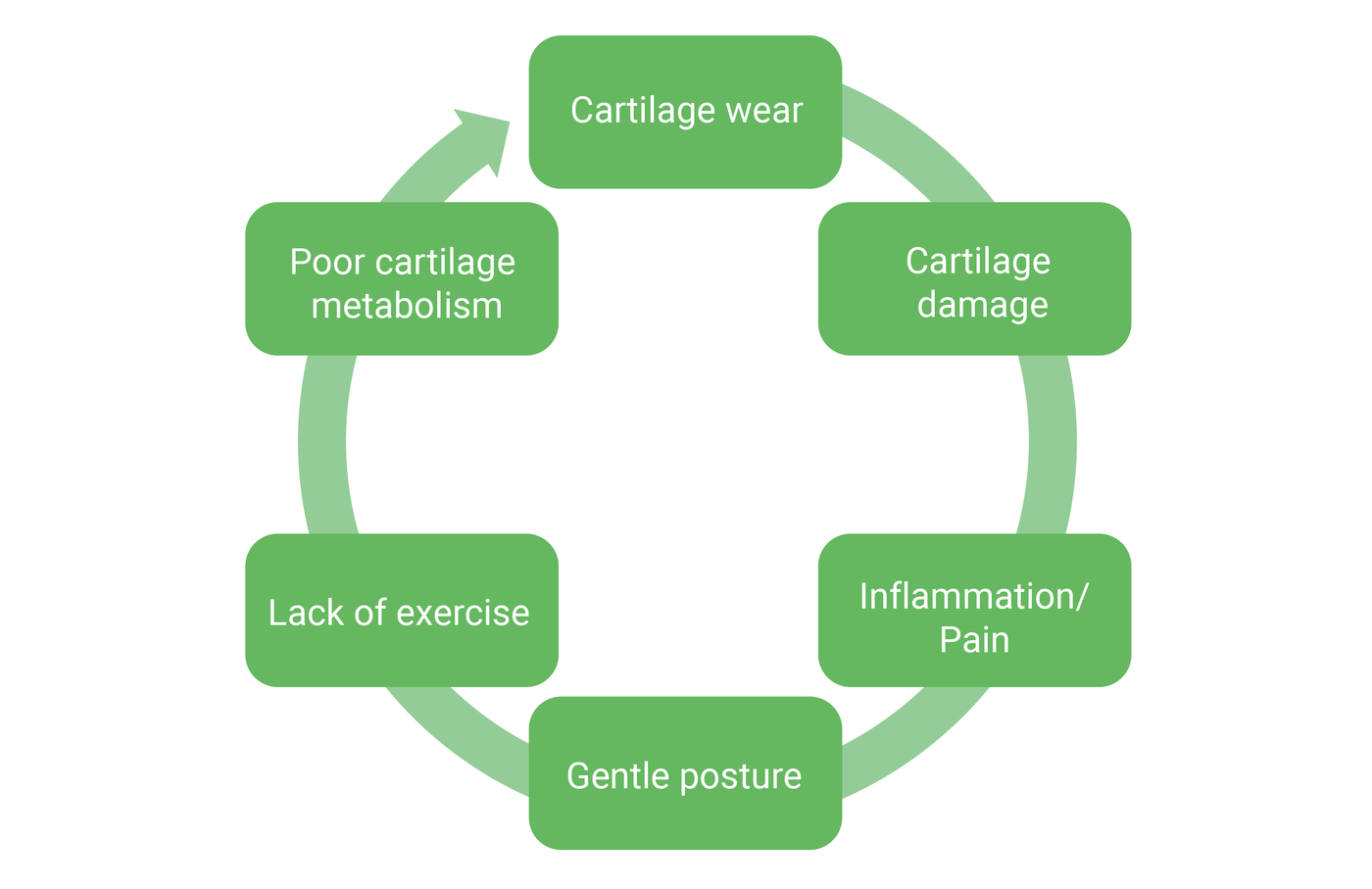
The vicious circle of arthrosis: the symptoms as the causes of the complaints
With osteoarthritis, symptoms that occur over a longer period of time can also become the causes of the complaints. The wear and tear on the cartilage leads to cartilage damage, which triggers inflammation and pain. Due to the pain, the patient adopts a protective posture, which leads to a lack of movement. The lack of movement in turn causes the cartilage metabolism to deteriorate, which further fuels the cartilage wear and aggravates the complaints. The so-called vicious circle of arthrosis is closed.
Dr Gottlieb, MD, the specialised foot surgeon in Berlin advises:
"In principle, arthrosis is the result of a persistent mismatch between load and load-bearing capacity. Too much or too little exercise also plays a role. Very active athletes, for example, can be just as affected as patients who hardly move at all and thus develop inactivity arthrosis. Sports that are easy on the joints, such as swimming or cycling, are recommended. Regular walks can also be helpful."
What causes arthrosis in the foot?
Arthrosis of the foot is usually caused by age due to wear and tear of the buffering cartilage layer in the affected joint (primary arthrosis). However, accidental injuries, fractures, overuse in sports and incorrect stresses at work or in everyday life can also trigger arthrosis in the foot at a younger age (secondary arthrosis).
Primary arthrosis can develop due to ageing
The risk of osteoarthritis increases with age. Around 50 % of all women over the age of 60 and one third of all men are affected by this joint-wasting disease. In the age group of over 70 years, arthrotic joint changes are found in about 80 % of all women and men. Age-related arthrosis in the foot is also called primary arthrosis and is caused by wear and tear of the joint cartilage. The cause is often many years of overuse or incorrect loading. Diseases such as osteoporosis, obesity, rheumatism or gout, which are typical diseases of old age, can additionally accelerate the course of arthrosis in seniors.
Secondary arthrosis is the result of accidental injury or incorrect stresses
If arthrosis develops due to factors unrelated to age, it is called secondary arthrosis. If joint wear occurs at a younger age, for example, the causes are usually accidental injuries or incorrect stresses. Extreme sporting stress or incorrect posture in everyday working life can therefore be causes of secondary arthrosis. Severe, permanent overweight can also put excessive strain on the weight-bearing joints and trigger secondary arthrosis.
Difference between arthritis and arthrosis:
Arthritis is the inflammation of a joint. Arthrosis, on the other hand, describes joint wear and tear. However, with arthrosis there are recurring inflammatory conditions of the joints (arthritides).
How the Doctor diagnoses arthrosis in the foot
Dr Tonio Gottlieb, MD as a specialist in foot and ankle surgery, can often already make the diagnosis “arthrosis” if the characteristic symptoms are present and on the basis of the orthopaedic examination. To confirm the diagnosis, an additional X-ray examination or magnetic resonance imaging (MRI) can be performed. These imaging methods allow a precise determination of the condition of the arthrosis in the foot.
The most important examination methods for diagnosing arthrosis of the foot are:
- Orthopaedic examination: By palpating and checking the range of motion of the foot joints, the doctor can determine how far the arthritic joint disease has progressed.
- X-ray examination: A conventional X-ray examination of the feet while standing can confirm a change in the joint space and bony outgrowths at the joint (osteophytes).
- MRI (magnetic resonance imaging): An MRI is helpful to better assess the condition of the joint cartilage. MRI images soft tissue such as cartilage, joint capsule, tendons, ligaments and muscles using a magnetic field and radio waves.
- Blood test: If there are pronounced signs of inflammation or a rheumatic disease is suspected, the cause of the arthrosis can be further narrowed down by a blood test.
After a detailed examination, the foot surgeon Dr Tonio Gottlieb, MD can tell you exactly which treatment methods are most suitable for you in the event of foot arthritis. Dr Gottlieb, MD is not only an experienced foot surgeon, but also actively researches all aspects of foot health. This means that he can always treat his patients according to the latest scientific findings. Make your personal consultation appointment at the specialist's practice right away!
In these cases, the foot surgeon considers an operation for arthrosis in the foot to be advisable
Whether one should operate on arthrosis in the foot depends on the stage of the disease and the degree of the respective complaints. If the degree of suffering is very high and mobility is correspondingly limited, the patient should consider surgical intervention. A timely operation can also prevent the arthrosis from spreading further and neighbouring joints from being progressively damaged. In the early stages of arthrosis, it is also possible to save the joints by correcting their position surgically without fusing them.
These surgery options are available
- arthroscopy (joint endoscopy, also joint lavage): In certain cases - mostly in the early stages of arthrosis - protruding tissue, pieces of cartilage and bone can be removed arthroscopically. This is a minimally invasive procedure using a special endoscope.
- position correction: If there is primary arthrosis due to a foot malposition, the axial malposition itself can be corrected surgically and the joint can be preserved.
- Arthroplasty: Arthroplasty is one of the joint-preserving operations. Bony protrusions or disturbing bone protrusions at the joint (osteophytes) are surgically removed and the bone friction is thus reduced.
- arthrodesis (joint fusion): With this surgical option, the joints are stabilised by "stiffening". For this purpose, the remaining cartilage is removed from the joint space and the damaged joint is then fixed with screws or plates. Arthrodesis can eliminate pain in the joint, stabilise an unstable joint or correct a deformed joint. The patient can move his or her foot almost normally again because the mobility of the adjacent joints is maintained. Extension, flexion and rotational movements are still possible, so that walking, driving, hiking or jogging is not impaired.
- joint replacement (prostheses): The fifth option for effectively treating foot arthrosis is the use of an artificial joint. However, this surgical method is only considered for very selected indications.
What is the healing process like after the surgery?
The healing process after an operation always depends on the course of the operation and the surgical technique used. For an initial overview, it is useful to distinguish between operations after which full weight bearing or partial weight bearing is possible.
- arthroscopy (joint endoscopy) = full weight bearing
- position correction = full or partial weight bearing
- arthroplasty = full weight bearing
- arthrodesis (joint stiffening) = full or partial weight bearing
- reconstruction of foot statics = mostly partial weight bearing
- joint replacement (prostheses) = partial weight bearing
Healing process for stress-stable interventions (full weight bearing is possible)
As a rule, all outpatient procedures can be classified as load-stable. However, an arthroscopy or position correction can also be stable. In this case, the first weight-bearing of the foot or even full weight-bearing is possible directly after the operation - depending on the symptoms.
As a rule, the patient has to wear a walking aid after the surgical intervention. This so-called orthosis (orthopaedic shoe or boot) serves to stabilise and relieve the operated foot. It is worn until the foot has completely healed and the transition to a ready-made shoe is possible. Here, too, the duration of wear depends on the type and extent of the operation.
Healing process for exercise-stable interventions (only partial weight bearing is possible)
Exercise-stable interventions include all operations to reconstruct the statics of the foot, the tarsus and the ankle joint, as well as some arthrodesis (joint fusion) and prostheses.
After the operation, the patient is put in a cast for about two weeks. During this period walking is only possible with ground contact and a walker. After removal of the cast, a so-called "walker" is individually fitted. This removable foot orthosis supports the rehabilitation after the operation and must be worn for about six weeks, in some cases even longer.
Already two weeks after the operation, the patient may start with targeted foot gymnastics exercises as part of physiotherapy. This promotes the mobility of the foot and restores it in the long term.
"After a pure arthroscopy, for example, the patient can perform again immediately. In the case of extensive arthroscopic surgery, you have to reckon with a longer relief phase. After reconstruction the operated foot can be fully or partially weight-bearing again immediately, depending on the case. The latter means that it can already be moved, but not yet loaded."
To the appointment
When are conservative treatment options for arthrosis of the foot really promising?
Conservative treatment measures can offer help with arthrosis of the foot, especially in the early stages. In principle, however, arthritic joint wear and tear cannot be cured by conservative therapy methods. The impairments and pain caused by arthrosis of the foot can only be remedied by stabilising the affected joint. This is usually done by arthrodesis (joint fusion).
Two conservative (non-surgical) therapies offer help for the onset of arthrosis in the foot:
- relief of painful joints, e.g. through orthopaedic shoe insoles.
- increasing resilience through physiotherapy (physical therapy)
The supportive foot orthosis is the most common conservative therapy method
Orthopaedic shoe insoles or shoe fitting are one of the most common recommendations in conservative therapy for arthrosis of the foot. These are made so specifically and precisely that the joints affected by the arthrosis are relieved as much as possible.
Physiotherapy can increase the resilience of the joints
Targeted gymnastics for arthrosis of the foot helps to increase the load-bearing capacity of the ankles and to strengthen the muscles. Physiotherapeutic training with special, regular exercises can stop the progression of arthrosis.
Can arthrosis in the foot be prevented?
Age-related arthrosis cannot be stopped. About 80 % of all men and women over the age of 70 are affected by this degenerative joint disease. Nevertheless, it is possible to take precautions at a younger age to prevent the development of arthrosis in the foot.
Tips for preventing arthrosis in the foot:
- Pay attention to the body's warning signs of overloading and incorrect loading: Anything that puts a lot of strain on the ankles or even causes pain should be avoided. However, under no circumstances should you adopt a protective posture. Susceptible joints in particular need exercise.
- Have malpositions treated and corrected at an early stage: Congenital foot malpositions such as a cavus or flat foot can lead to the development of arthrosis over the years and should be treated in good time with orthopaedic insoles and gymnastic exercises.
- Pay attention to the correct behaviour when walking: Misuse and overloading also result from incorrect walking behaviour. In physiotherapy, you can learn how to counteract this incorrect behaviour.
- Let injuries and fractures heal: Secondary osteoarthritis of the foot often develops after injuries or fractures. In this case, it is important to have fractures treated correctly by a foot surgeon.
- Healthy diet: Being overweight can promote the development of osteoarthritis. It is therefore advisable to avoid or reduce excessive weight by eating a balanced, healthy diet.
- Avoid excess weight: Excess weight is a risk factor for the development of arthrosis in the foot, as the joints are put under additional strain by excess pounds. To prevent this, one should therefore pay attention to a healthy body weight.
- Suitable footwear: Choosing suitable, comfortable everyday shoes is important for the prevention of osteoarthritis. The right sports shoes should also be selected depending on the type of sport. Special arthrosis shoes are characterised by a rounded shape that is stiffened in the forefoot area. This relieves pressure points and prevents buckling in the forefoot area.
- Regular and gentle exercise: Daily walks or bike rides promote joint mobility and are gentle on the joints at the same time.
Are you looking for an experienced orthopedic foot and ankle surgeon to treat arthrosis of the foot? Are you wondering whether conservative therapy is sufficient or whether surgery is necessary? Would you like to get a second opinion on your orthopaedist's recommendation for surgery? The foot surgeon Dr. Tonio Gottlieb has extensive specialist knowledge and many years of experience in the treatment of all kinds of foot diseases. Whether conservative therapy or foot surgery, he finds the optimal solution for every foot problem - make a consultation appointment right away!
Make an appointment with Dr Gottlieb, MD




